Understanding Why Your Leg Feels Disconnected From Your Hip

Medically Reviewed By:
Feeling like your leg is disconnected from your hip can be unsettling and disruptive to daily life. This sensation may indicate an underlying issue involving the hip joint, the surrounding muscles, or the nerves that support leg movement and stability.
Addressing this sensation is crucial because the hip joint maintains balance and mobility. Ignoring these symptoms could result in further complications, including chronic pain, reduced range of motion, or difficulty performing daily tasks. Identifying the underlying cause may help in exploring management options.
The Sacroiliac Joint’s Role In Leg And Hip Connection
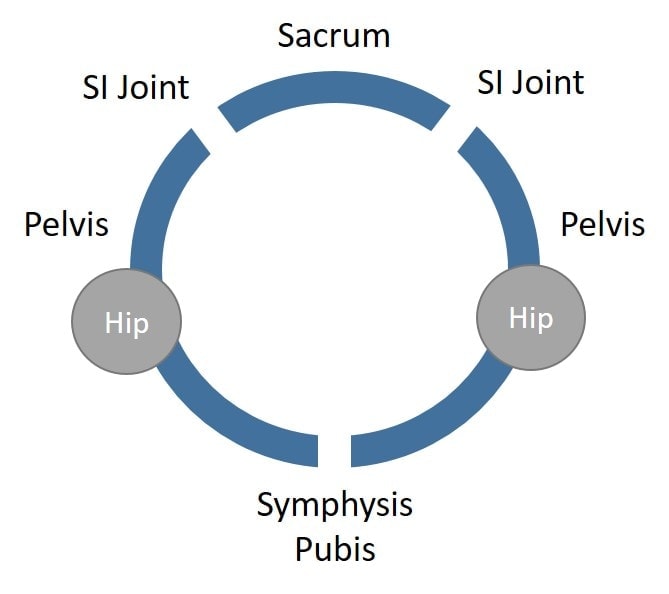
The sacroiliac (SI) joint is an anatomical structure where the tailbone (sacrum) connects to the back of the hip bone (ilium). Along with the symphysis pubis at the front of the pelvis, it forms part of a three-joint system known as the pelvic ring. These joints work together to transfer forces between the spine and the lower limbs, bridging movement and stability.
The SI joint ensures stability while allowing subtle movements essential for walking, running, and other activities. It functions alongside strong ligaments and surrounding muscles to absorb shock and distribute weight evenly. The SI joint facilitates smooth motion and supports balance and posture by connecting the upper body and legs.
Associated Symptoms Of Leg Instability
Leg instability often presents as weakness or unsteadiness when bearing weight or moving. This unsettling experience can make everyday activities, such as walking or climbing stairs, more difficult. It is commonly accompanied by additional symptoms that may help identify the underlying cause. These associated symptoms include:
Lack Of Support In The Leg
A lack of support in the leg may feel as though the leg cannot bear weight or maintain stability. This sensation often results from weakened muscles, nerve dysfunction, or joint instability, which impair the leg’s ability to provide the strength and balance required for movement.
Even simple tasks like standing, walking, or climbing stairs can become challenging or unsafe when the leg feels unsupported. This instability often leads to compensatory movements, which can strain other body areas, including the hip, back, or opposite leg. Over time, these compensations may contribute to additional pain, reduced mobility, and an increased injury risk.
Difficulty Standing Or Walking Steadily
Struggling to stand or walk steadily is a common symptom of leg instability and can significantly disrupt daily activities. This difficulty often stems from issues affecting the muscles, joints, or nerves that maintain balance and coordination. For example, weakened muscles in the hip or leg, joint dysfunction, or nerve compression can interfere with the body’s ability to distribute weight evenly and stay stable.
This challenge may manifest as wobbling, swaying, or the sensation that the leg might “give out” while bearing weight. Over time, these issues can lead to compensatory movements, increased fatigue, or a heightened risk of falls. Additionally, difficulty walking steadily is often accompanied by symptoms such as pain, stiffness, or numbness, which can further limit mobility.
Pain, Swelling, Or Redness In The Joint
Pain, swelling, or redness in a joint often indicates inflammation or injury, contributing to leg instability. These symptoms are commonly associated with joint sprains, arthritis, or bursitis. However, they may also suggest underlying issues such as infection or trauma.
Joint pain can range from mild discomfort to sharp, debilitating sensations, particularly during movement or weight-bearing activities. Swelling often results from fluid accumulation in the joint, which may limit mobility and exacerbate stiffness. Redness, when present, typically signals increased blood flow as the body responds to irritation or damage in the area.
Numbness
Numbness in the leg or hip can be a concerning symptom, often signaling nerve involvement. This loss of sensation occurs when the nerves transmitting signals between the brain and lower body become compressed, damaged, or irritated. Common causes include sciatica, herniated discs, or nerve entrapment in the hip or pelvic region.
Numbness may present as a complete lack of feeling or as a dull, tingling sensation, making it difficult to perceive pressure, temperature, or pain in the affected area. It may appear on its own or accompany other symptoms, such as weakness, instability, or a pins-and-needles sensation.
Muscle Spasms
Muscle spasms are involuntary contractions that may cause sudden, sharp pain and tightness in the leg or hip. These spasms often arise from muscle fatigue, overuse, dehydration, or irritation of the nerves controlling the affected muscles. They may also result from underlying issues such as nerve compression, joint instability, or poor circulation.
Spasms can range from brief and mild to prolonged and severe, potentially interfering with movement or weight-bearing on the affected leg. In some cases, they may be accompanied by stiffness, tenderness, or visible muscle twitching. Repeated spasms can worsen feelings of instability and increase strain on surrounding joints and tissues.
What Causes The Sensation Of A Leg Disconnected From The Hip?
The sensation of a leg disconnected from the hip can be alarming. It may indicate an issue with the structures connecting these areas. Several factors can disrupt the interaction between the hip joint, surrounding muscles, and nerves, resulting in this unsettling feeling. Identifying the possible causes is essential for pinpointing the source of the problem and pursuing effective solutions. Common causes include:
- Nerve Problems: Nerve issues like herniated discs disrupt signals between the brain and leg, causing weakness, numbness, and instability.
- Muscle Weakness: Weak hip muscles, like glutes and flexors, can destabilize the leg, causing instability, limited motion, and a disconnected sensation.
- Hip Impingement: Femoroacetabular impingement (FAI) occurs when abnormal contact between the hip joint’s ball and labrum causes pain, stiffness, and instability.
- Sciatica: Sciatica is nerve compression causing sharp pain, tingling, or weakness from the lower back to the leg, often making movement difficult and unstable.
When To Seek Medical Attention
Leg instability can sometimes improve with rest and strengthening exercises, but professional evaluation should be pursued if you experience any of the following:
- Persistent instability or frequent episodes of the leg “giving out.”
- Severe pain in the hip, knee, or lower back accompanying the instability.
- Tingling, numbness, or a loss of sensation in the leg or foot.
- Swelling, redness, or warmth around a joint—as this may indicate inflammation or infection.
- Difficulty bearing weight or walking without assistance.
- A recent injury or trauma that caused the instability.
- Loss of sensation in the groin
- Loss of bowel and/or bladder control
- Worsened balance and/or coordination
If symptoms worsen over time or interfere with daily activities, speaking with a healthcare professional is vital to identify the root cause and prevent further complications. Early intervention is key to restoring stability and improving mobility.
Diagnosing Hip And Leg Instability
Diagnosing hip and leg instability requires a comprehensive evaluation to identify the underlying cause and create an effective treatment plan. Physicians typically begin by taking a detailed patient history, exploring symptoms, recent injuries, activity levels, and any pre-existing conditions that might contribute to instability.
A physical examination follows, during which the physician evaluates the range of motion, strength, and stability of the hip and leg. They may also check for swelling, tenderness, or misalignment. Diagnostic imaging is often recommended to examine the affected structures more closely if further investigation is needed. Standard imaging techniques include:
- X-rays: Used to detect fractures, bone deformities, or arthritis in the hip or leg joints.
- MRI: Provides detailed images of soft tissues, such as ligaments, muscles, and nerves, to identify tears, inflammation, or compression.
- CT scan: Offers cross-sectional images for a comprehensive view of bones and surrounding tissues, particularly useful after trauma.
By combining diagnostic tools with physical exams and patient history, physicians can determine the root cause of instability and develop tailored treatment options. Early and accurate diagnosis is crucial for effectively addressing symptoms and preventing complications.
Conventional Treatment Options
Traditional care for hip and leg instability focuses on relieving symptoms, promoting healing, and restoring function through non-surgical methods. Depending on the cause and severity of the instability, commonly used approaches include:
- Immobilization: Braces, splints, or slings may be recommended to stabilize the joint, prevent further injury, and allow tissues to heal.
- Physical therapy: Targeted exercises and stretches strengthen muscles, enhance joint stability, and restore mobility while reducing pain.
- Traction: For cases of nerve compression or joint misalignment, traction may relieve pressure, improve alignment, and support better function.
- Medication: Over-the-counter pain relievers, anti-inflammatory drugs, or muscle relaxants can help manage discomfort and swelling.
- Localized injections: Corticosteroid or hyaluronic acid injections are sometimes used to help manage inflammation and discomfort. However, repeated use may carry risks, such as tissue damage or joint degeneration, and should be carefully considered.
These treatments are often used as a first-line approach before considering surgical intervention and may be explored for their potential role in managing instability.
Exploring Non-Surgical Options For Hip And Leg Instability
Physicians in the licensed Regenexx network offer non-surgical procedures that use Regenexx lab processes and proprietary injectates to support joint function and promote improved stability. These procedures, which may include platelet-rich plasma (PRP) injections, are typically part of a broader, customized care approach designed to address underlying contributors to joint instability without the need for surgery.
- Platelet-Rich Plasma (PRP) Procedures – In a procedure using Regenexx lab processes and proprietary PRP injectates, a physician in the licensed Regenexx network isolates growth factors from the patient’s own blood and injects them into the targeted area under image guidance. This approach may help support ligament health and joint stability.
PRP injections may be administered around the sacroiliac (SI) joint, symphysis pubis joint, and other supporting musculoskeletal structures using fluoroscopy-guided placement.
In some cases, PRP may also be used to address specific spine-related nerve conditions, as well as certain soft tissue or hip joint issues that could contribute to sensations of instability in the leg, such as a feeling of the leg giving out or being disconnected.
While corticosteroid injections are sometimes used for short-term symptom relief, repeated use may carry risks. Interventional orthobiologic procedures are being explored for their potential role in supporting joint integrity and mobility.

Medically Reviewed By:
