5 Questions About Hip Arthroscopy for Hip Impingement
Hip arthroscopy for hip impingement or a labral tear is more invasive than you’ve been led to believe. Add to that a laundry list of side effects and the wealth of research showing poor results, especially in patients with arthritis, and you have to wonder why anyone chooses to go through it. If you are considering hip arthroscopy, we have answered 5 questions about hip arthroscopy for hip impingement that should provide more clarity as you make your decision. First, let’s get familiar with hip anatomy.
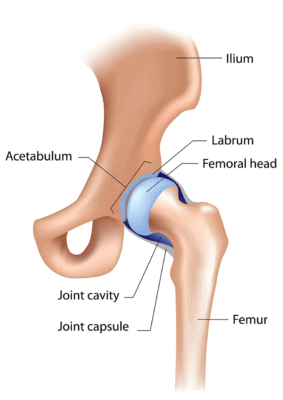
Alila Medical Media/Shutterstock
The Anatomy of a Hip
The hip is a ball-and-socket joint. The ball forms the head of the femur and when functioning optimally fits nicely into the socket, a bowl-shaped depression in the hip bone called the acetabulum. The acetabulum is lined with cartilage to cushion the joint, and there is a fibrous lip around the socket called the labrum. All of these structures can be affected when there is a hip impingement.
1. What Is Hip Impingement?
Hip arthroscopy for hip impingement is a common indication for the surgery. The medical term for this is femoroacetabular impingement (FAI). This means there is a bone spur either on the socket (pincer impingement) or the ball (cam impingement) of the joint or on both. A bone spur is just an extra growth of bone.
Surgeons typically advise that bone spurs be removed because early studies showed that the spur was associated with hip arthritis. But the key thing missing from the studies was how they are associated. A large study specifically looking at impingement and osteoarthritis answered the how by showing that the spur formed to protect the joint and that patients who had it developed less arthritis over time. So instead of causing arthritis, the bone spur protected against it! This means that by cutting out the bone spurs, the surgeon is removing the body’s natural response to protect itself from arthritis. Hip bone spur removal is a bad idea!
The labrum can also become torn or frayed, which when combined with hip pain is also considered an indication for arthroscopy. During arthroscopy the torn piece of the labrum can be cut out or an attempt can be made to rebuild it. Hip arthroscopy surgeries for labral tears when hip arthritis is also present also tend to be unsuccessful.
2. Does a Hip Impingement Cause Pain?
If an impingement or a labral tear was a common source of hip pain, we would expect that patients without hip pain wouldn’t have these findings and patients with hip pain would be the only patients who have them.
The traditional orthopedic thinking that leads to surgery is that a small number of us are born with hips that tend to “impinge,” and this extra wear and tear can rapidly lead to arthritis. As a result, if someone has an MRI showing hip impingement and also has hip pain, he or she must need an invasive surgery.
However, what if your pain had nothing to do with the hip impingement? What if I told you that the research shows that just about everyone, whether they have pain or not, has a hip impingement? A Norwegian study looked at 2,081 young adults with X rays of their hips. Surprisingly 97.1% of the men and 98.6% of the women had at least one X-ray finding of hip FAI! Yes, almost everybody had hip FAI!
So almost everyone has some degree of hip impingement and most of us never even know it because we never have pain. So if we have hip pain, and the results of our MRI show a hip impingement, is it the impingement causing our hip pain or could it actually be something else? Do we really want to undergo an invasive hip arthroscopy if impingements are also common in patients without pain and arthritis? The answers, respectively, are, yes, it could be something else causing your hip pain—perhaps the problem isn’t really in your hip—and, no, we should look for alternatives.
3. If I Have Arthritis with My FAI: Should I Have a Hip Arthroscopy?
No. But, unfortunately, many hip arthroscopy patients we’ve evaluated after failed surgeries had evidence of arthritis before their procedure, even though surgery on patients with hip arthritis has been shown time and time again to be unsuccessful.
In a new study, researchers looked at the records of all of the patients from one hospital who had hip arthroscopy for hip impingement. Two groups were established: a group whose records reflected arthritis or bone involvement and a control group whose records showed no evidence of this. The study concluded that surgery for a torn labrum with impingement will be significantly less successful with the presence of any arthritis or bone involvement. This is true even in mild cases of arthritis.
4. What Are the Side Effects of Hip Arthroscopy?
There are many side effects to hip arthroscopy. We all conceptualize that arthroscopy is “minimally invasive” because it’s less invasive than an open surgery. However, hip arthroscopy is much more invasive than knee arthroscopy. Here are some side effects:
- Worsening arthritis: In this study, the authors found that even the smallest evidence of arthritis at the time of surgery dramatically reduced outcomes with almost 6 in 10 having worsening arthritis as a result of the surgery. This seems to hold up based on the fact that the bone spurs often removed by hip arthroscopy surgery for impingement are no longer able to protect the cartilage.
- “The Portal Syndrome”: This is chronic pain from the portals used for hip arthroscopy. The portals are the tunnels created so they can put the ball-point-pen-sized hip arthroscope into the joint. We’ve seen nerves become entrapped in these portals, and to relieve the pain, we’ve used platelet lysate (growth factors from a patient’s own blood platelets) to hydrodissect (via an ultrasound-guided injection) the small nerves in the portals.
- Nerve damage: During arthroscopy major traction has to be pulled on the hip to allow room for the hip arthroscopy instruments. How much traction? An awful lot! So much so that the major nerve of the leg and thigh (the femoral nerve) frequently loses the ability to transmit signals during the surgery.
- Metal debris: We’ve seen it in almost all joint replacements that have any type of metal component, but metal debris is also being left behind in arthroscopies. In this case a team of researchers took a metal bone shaver of the type used in hundreds of thousands of joint arthroscopy surgeries annually. They shaved some bone pieces and then looked under a microscope and saw a significant amount of metal debris created by the bone shaver. They also noted that these metal particles killed off some joint cells. In addition, they caused the synovial cells of the joint to produce nasty toxic cytokines that could harm the joint.
5. Are There Alternatives to Hip Arthroscopy for Hip Impingement?
Yes! We treat hip impingement patients first by trying to remediate the biomechanical hip issues that caused the bone spur to form. You would be surprised at the damage bad biomechanics can do and equally surprised at how easy it is to correct. Second, we support hip-joint cartilage health by injecting highly concentrated platelets or stem cells into the joint.
The upshot? Hip arthroscopy has been the fastest growing orthopedic surgery for over a decade. Prior to that, outside of a few procedures, hips couldn’t be operated on without a hip replacement. While this may seem like a medical advance, unnecessary hip arthroscopies, because they are labeled as “minimally invasive,” are being divvied out like Band-Aids. We hope our questions will lead you to the right decision if you are considering hip arthroscopy. As the very least, if you have arthritis with hip impingement, please look for other alternatives. Also think twice about this invasive surgery if you don’t have arthritis. If you have to have it, at least make sure you exhaust your nonsurgical treatment options as described above, which consist of more than just a steroid shot in the hip!
Can a stem cell procedure help me? To find out if you might be a candidate for a Regenexx stem cell procedure, complete our Regenexx Procedure Candidate Form online.

NOTE: This blog post provides general information to help the reader better understand regenerative medicine, musculoskeletal health, and related subjects. All content provided in this blog, website, or any linked materials, including text, graphics, images, patient profiles, outcomes, and information, are not intended and should not be considered or used as a substitute for medical advice, diagnosis, or treatment. Please always consult with a professional and certified healthcare provider to discuss if a treatment is right for you.
