Considering Spinal Fusion For Back Pain? Know The Facts

Medically Reviewed By:
Spinal fusion permanently connects two or more vertebrae using hardware and bone grafts to stabilize a portion of the spine. While surgeons often recommend this procedure for spinal instability or persistent back pain, it carries potential risks and long-term considerations.
Research suggests that spinal fusion does not always lead to long-term pain relief or improved function. Some individuals may continue to experience discomfort and limited mobility following the procedure. Before considering this approach, exploring all available options and understanding the potential outcomes is vital.
Why Understanding the Spine Is Critical for Fusion Outcomes
Evaluating spinal fusion as a treatment option requires a clear understanding of how the spine functions.
The spine is a complex structure that provides support and mobility. It consists of vertebrae stacked like building blocks, forming a stable framework while protecting the spinal cord. Discs between the vertebrae function as shock absorbers, aiding in impact distribution and preserving flexibility.
Facet joints regulate movement between vertebrae, while ligaments and muscles—particularly the multifidus—help stabilize the spine. The spinal cord, a bundle of nerves within the spinal column, transmits signals between the brain and body to coordinate movement and sensation. The spine’s natural curves assist in distributing weight, supporting balance and function.
Watch the video below for a detailed explanation of the spine’s structure and function.
What Is Spinal Fusion?
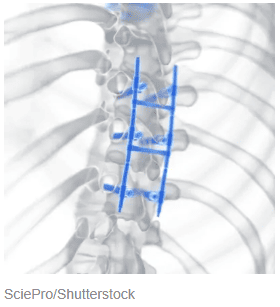
Spinal fusion is a surgical procedure that permanently joins two or more vertebrae to help stabilize the spine. One common approach, a 360-degree fusion, involves securing the vertebrae from both the front and back of the spine. Physicians may recommend fusion for conditions such as degenerative disc changes, herniated discs, spinal stenosis, and instability.
These procedures are typically extensive and may involve a prolonged recovery period. Although surgeons perform spinal fusion to improve stability, long-term outcomes can vary, with some individuals continuing to experience discomfort or limited mobility following surgery.
How Is Fusion Surgery Performed?
Spinal fusion surgery uses hardware and bone grafts to help stabilize the spine. The procedure typically involves the following steps:
- Anesthesia and incision: The patient receives general anesthesia. The surgeon makes an incision in the front (anterior approach), back (posterior approach), or both (360-degree fusion).
- Disc and tissue removal: The surgeon removes the affected disc or soft tissue between the vertebrae to create space for the nerves at the level of concern.
- Bone graft placement: A bone graft from the patient (autograft), a donor (allograft), or synthetic materials is placed between the vertebrae to support fusion.
- Hardware placement: Screws, rods, or plates may be secured to the vertebrae to help maintain stability.
- Closure and recovery: The surgeon closes the incision, and the patient begins a recovery process as the bones gradually fuse, which may take several months to a year.
Recovery Process
Recovery after spinal fusion can take several months and requires ongoing monitoring. Most individuals remain in the hospital for about four days, though some may require a longer stay. Some patients with ongoing mobility or medical issues may require a transfer to a rehabilitation facility for intensive therapies before going home. During this time, medical staff monitor patients, often using devices such as a heart monitor, IV, or catheter.Once discharged, follow-up appointments are necessary to assess healing and monitor for potential complications. Physical therapy is recommended to improve mobility and strength, though progress may vary. Some individuals experience stiffness or discomfort during recovery, which can affect their ability to return to previous activity levels.
Conditions Treated With Spinal Fusion Surgery
Spinal fusion is often recommended for conditions that cause instability, pain, or structural issues in the spine. Below are some common conditions for which spinal fusion is considered.
- Bulging disc: A bulging disc occurs when a spinal disc extends beyond its normal space without rupturing. Depending on the affected area, it may cause localized pain or nerve compression, leading to numbness, tingling, or weakness in the back, neck, or limbs. Read More About Bulging Discs.
Associated Risks Of Spinal Fusion Procedures
Spinal fusion involves surgical intervention to stabilize the spine, and like any procedure, it carries potential risks. The surgery alters the natural movement of the spine, which may contribute to complications during and after the procedure. Below are some considerations for different types of spinal fusion:
- Posterior lumbar interbody fusion: Various surgical approaches—including posterior, anterior, and lateral fusion—may involve risks such as bone graft complications, nerve irritation, or increased stress on adjacent spinal segments.
- Anterior lumbar interbody fusion: Approaching the spine from the front may involve a risk of affecting nearby blood vessels, which could lead to increased blood loss or other complications.
Fusion Procedures May Lead to Adjacent Segment Disease
Spinal fusion alters natural spinal movement, which may increase stress on vertebrae above and below the fused section. This additional strain can contribute to adjacent segment disease (ASD), a condition where nearby spinal segments degenerate over time.
When one section of the spine loses mobility, adjacent vertebrae may compensate, potentially leading to degenerative changes such as arthritis, disc damage, or instability. Even when fusion achieves its intended goal, ASD remains a possible long-term concern and may contribute to pain, mobility challenges, or the need for additional procedures.
Study Shows Serious Issues With 360-Degree Lumbar Fusions
One 2016 study examined 360-degree lumbar fusions in 73 patients at 2, 5, 10, and 15 years post-surgery. While early outcomes appeared positive, long-term data suggested a decline in patient-reported results. The study noted a high occurrence of ASD and frequent revision surgeries:
- 5 years post-op: 7 patients underwent revision surgery.
- 10 years post-op: 18 patients underwent revision surgery.
- 15 years post-op: 24 patients underwent revision surgery.
By 10 years post-surgery, radiology exams identified ASD in 51% of patients, leading researchers to evaluate the long-term effects of this procedure. Between 10 and 15 years, disability scores returned to pre-surgery levels, aligning with some clinical observations.
While some studies suggest genetic factors may contribute to ASD, research indicates that spinal fusion itself may play a role in accelerating degeneration over time.
Additional Complications And Effects To Consider
Spinal fusion is an extensive surgical procedure that carries potential risks. Patients may experience:
- Blood clots: Increased risk of deep vein thrombosis or pulmonary embolism.
- Infection: Surgical site infections may require additional treatment.
- Bleeding: Excessive blood loss can affect recovery.
- Pain: Some individuals experience persistent or worsening pain.
- Anesthesia risks: Possible complications include breathing issues or adverse reactions.
- Nerve injury: May lead to weakness, numbness, or functional changes.
- Tingling or numbness: Common in the legs due to nerve involvement.
- Loss of movement: Rare but possible with nerve or spinal cord damage.
- Bone graft concerns: Donor grafts may carry risks of infection, rejection, or poor integration.
Even when spinal fusion is considered successful, pain relief is not guaranteed. Some individuals continue to experience discomfort or limited improvement following surgery.
Is Fusion Surgery Worth It? Evidence Suggests Otherwise
Spinal fusion may be considered in cases of severe instability, though these situations are uncommon. Some individuals who undergo fusion require additional surgeries, long-term pain management, or experience complications such as changes to the multifidus muscle—a key stabilizer of the spine. Despite the invasiveness and cost of the procedure, long-term benefits remain inconsistent..
Research supporting spinal fusion remains mixed. While some studies report positive outcomes, others highlight challenges such as ongoing pain, mobility limitations, and a high occurrence of ASD. Funding sources, including device manufacturers, may influence study results, underscoring the need for independent research.
For conditions such as spinal stenosis, fusion surgery may carry greater risks than decompression procedures, which have become more common alternatives over the past two decades. Given the potential risks and varying outcomes, exploring all available treatment options is essential before considering fusion.
The Regenexx Approach Is An Alternative To Avoid Surgery Risks
Spinal fusion may involve a long recovery period, potential complications, and the possibility of ongoing pain. Procedures using Regenexx lab processes provide a less invasive option designed to support the body’s natural healing process and help improve function without the need for fusion.
Procedures using Regenexx lab processes utilize the body’s own healing components, such as platelet-rich plasma (PRP) and bone marrow concentrate, to target areas of damage, help reduce inflammation, and support recovery. These interventional orthobiologic treatments aim to support spinal mobility while offering an alternative to surgery.
Take Charge Of Spine Health With Fewer Risks Than Surgery
Spinal fusion is a common surgical approach, but its long-term effectiveness varies. Limiting spinal movement may place added stress on surrounding vertebrae, which can contribute to degeneration, discomfort, or the need for additional procedures.
Exploring less invasive, research-backed treatment options may help support recovery while supporting spinal mobility. Procedures using Regenexx lab processes utilize interventional orthobiologic approaches to promote healing and maintain function. Taking an informed approach to spine health helps individuals choose options that support long-term well-being.
Get started to see if you are a Regenexx candidate
To talk one-on-one with one of our team members about how the Regenexx approach may be able to help your orthopedic pain or injury, please complete the form below and we will be in touch with you within the next business day.

Medically Reviewed By:
