Arthroscopic Knee Surgery: Risks And Alternatives

Medically Reviewed By:
Arthroscopic knee surgery has traditionally been a common approach for addressing certain knee conditions, particularly meniscus tears. This procedure often involves identifying a tear through imaging and surgically removing the damaged portion of the meniscus.
Meniscus degeneration is known to contribute to knee arthritis, though the underlying mechanisms are not fully understood. For some middle-aged individuals with knee pain, meniscus surgery may not be the best option. Removing part of the meniscus can contribute to further joint degeneration, potentially worsening the condition rather than providing long-term relief.
Exploring Knee Anatomy
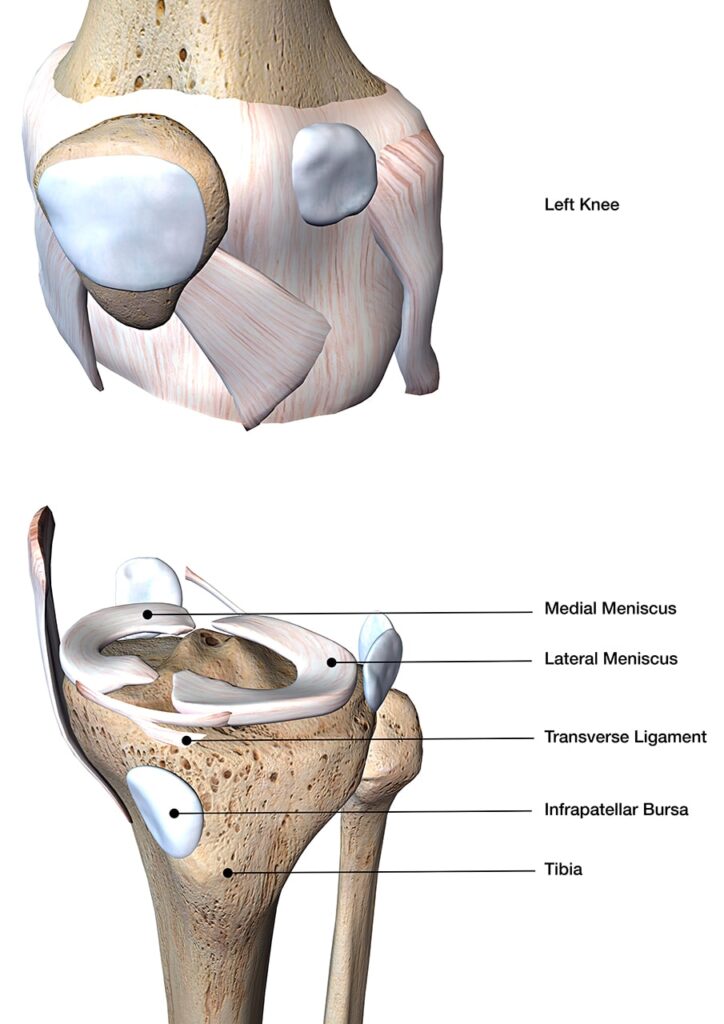
The knee is a complex hinge joint consisting of tendons, ligaments, cartilage, and bones that work together to provide mobility and stability. The primary bones forming the knee joint include the femur (thigh bone), tibia (shin bone), and patella (kneecap).
Positioned between the femur and tibia, the menisci are two crescent-shaped cartilage structures that cushion the joint during movement and help distribute weight evenly. Ligaments such as the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) contribute to knee stability, while tendons connect muscles to bones, thereby facilitating movement.
As a major weight-bearing joint, the knee relies on the integrity of these structures for proper function. Damage or degeneration of any component may lead to pain and impaired mobility, affecting overall joint health.
Who Is An Ideal Candidate For This Procedure?
Physicians may recommend arthroscopic knee surgery for individuals diagnosed with conditions such as meniscus tears, ligament injuries, or cartilage degeneration. When conservative treatments fail to provide relief from ongoing knee pain, reduced mobility, or mechanical symptoms like catching or locking, surgery may be considered as a next step.
Several factors influence the suitability of this procedure, including age, overall health, and activity level. Middle-aged individuals with degenerative knee conditions may be less likely to experience long-term benefits from surgery, particularly when the damage is associated with the natural aging process.
A comprehensive evaluation by a physician is essential to determine whether surgery is appropriate based on the specific knee condition and individual health considerations.
Arthroscopic Surgery For The Knee And How It Works
Arthroscopic knee surgery is a less invasive procedure for diagnosing and addressing knee conditions. Small incisions are made around the knee, allowing for the insertion of an arthroscope—a thin, flexible camera that provides a detailed view of the joint. This technique enables precise assessment and treatment of knee injuries.
In addition to visualization, specialized surgical instruments help address damage, such as trimming or removing tissue when necessary. The procedure is usually performed under local or general anesthesia and is often completed on an outpatient basis, allowing patients to return home on the same day.
Recovery time varies based on the extent of the procedure, with many individuals resuming light activities within a few weeks.
Success Rates—What The Research Says
A long-term study involving 119 patients who underwent arthroscopic partial meniscectomy reported favorable outcomes. At the four-year follow-up, 91.7% of patients rated their results as excellent or good. By the 12-year mark, 78.1% continued to report positive outcomes.
For individuals with isolated meniscal tears, early improvements were largely maintained over time. However, the study found that additional cartilage damage significantly affected long-term success. Among patients with both meniscal and cartilage damage, only 62% rated their results as excellent or good after 12 years.
Patients with untreated ACL ruptures also experienced poorer long-term outcomes. These findings suggest that while arthroscopic partial meniscectomy may provide short-term relief, the presence of additional joint damage can influence long-term effectiveness.
Conditions This Surgery Can Help With
Arthroscopic knee surgery can address various knee conditions affecting the cartilage, ligaments, and meniscus. Common conditions treated with this procedure include:
Surgical Meniscus “Repair” Frequently Involves Meniscus Removal
Meniscus “repair” surgery often involves removing the torn portion of the meniscus rather than preserving or restoring it. Many individuals undergo this procedure after a brief consultation with an orthopedic surgeon, expecting long-term relief.
Following surgery, a typical recovery plan includes rest, wearing a brace, and experiencing temporary symptom improvement.
Over time, symptoms may return, with knee swelling and additional cartilage damage appearing on follow-up imaging. In many cases, further surgery is recommended to remove more meniscus and cartilage, potentially leading to discussions about knee replacement.
Research indicates that meniscus surgery may be no more effective than a placebo, with no strong evidence supporting its long-term benefits. Removing portions of the meniscus reduces the joint’s natural cushioning, which may contribute to the progression of knee arthritis.
Additionally, eliminating damaged meniscus tissue may interfere with the joint’s ability to engage in natural healing processes.
Possible Complications Of This Knee Surgery
Although arthroscopic knee surgery is considered less invasive than traditional open surgery, it carries potential risks that may affect recovery and long-term outcomes. Complications can range from minor issues to more serious concerns, and understanding these risks is an important part of the decision-making process.
Possible complications of arthroscopic knee surgery include:
Risk Of Infection
Despite the small incisions used in arthroscopic knee surgery, there remains a risk of infection. Bacteria can enter the surgical site, potentially causing redness, swelling, pain, or fever. Further surgical intervention may be necessary to manage the infection and prevent complications in more severe cases.
Post-Surgical Pain And Stiffness
Pain and stiffness are common following arthroscopic knee surgery as the joint heals. The procedure can irritate the surrounding tissues, leading to temporary discomfort and restricted mobility. Pain is typically managed with prescribed medications, ice, and rest. However, stiffness may persist for several weeks or months as the knee gradually recovers.
Risk Of Blood Clots
Blood clots are a potential complication following arthroscopic knee surgery. Reduced mobility during recovery can increase the risk of clot formation in the veins, particularly in the legs. This may lead to deep vein thrombosis (DVT), which can cause swelling, pain, and other complications. Blood clots can also travel to the lungs, requiring immediate medical attention.
Potential For Nerve Damage
Nerve irritation or damage can occur during arthroscopic knee surgery, potentially leading to numbness, tingling, or weakness in the leg or foot. These effects are usually temporary and improve during the healing process. However, in rare instances, nerve damage may be more severe, resulting in long-term or permanent complications.
Long-Term Degenerative Effects
Arthroscopic knee surgery may contribute to the progression of degenerative changes within the joint. The removal of meniscus tissue, crucial in cushioning and stabilizing the knee, can increase stress on the cartilage and underlying bone. Over time, this added stress may accelerate the development of osteoarthritis or worsen preexisting joint degeneration.
Alternatives To Arthroscopic Knee Surgery For A Meniscus Tear
Recent research has raised questions about the necessity of surgery in certain cases of meniscus tears. For example, someone may experience knee pain during activities like hiking, followed by swelling and a “popping” sensation. Imaging might reveal a meniscus tear, leading to a surgical referral. However, studies suggest that the meniscus tear may not be the true cause of knee pain, and surgery may not always be required.
Physicians in the licensed Regenexx network offer procedures using Regenexx lab-processed injectates as a non-surgical option. These interventional orthobiologic procedures are designed to support the body’s natural healing processes and may assist in managing symptoms associated with meniscus-related knee pain.
For individuals not requiring urgent surgery, these procedures may be considered as part of a customized care plan.
Regenexx-SCP Injectates
Regenexx SCP (super concentrated platelets) is a specialized form of platelet-rich plasma (PRP) that concentrates the body’s natural growth factors. Physicians in the licensed Regenexx network utilize Regenexx SCP injectates to help promote tissue repair and manage inflammation.
These procedures may offer a less invasive alternative for individuals with meniscus-related symptoms and other knee conditions.
Regenexx-SD Injectates
Regenexx SD injectate is derived from a patient’s own bone marrow concentrate using Regenexx lab processes. This procedure involves a higher concentration of orthobiologic materials than standard approaches and is designed to support the body’s natural healing mechanisms for orthopedic tissue damage.
Preserve The Vital Role Of Your Meniscus
The knee meniscus is crucial to joint function, relying on specialized cells to maintain its structure and support mobility. Advanced imaging research shows that degenerative changes in the meniscus reduce the number of functional cells. When imaging detects a meniscus tear, the underlying degeneration—not necessarily the tear itself—often contributes to knee discomfort.
Surgical removal of meniscus tissue can further reduce joint support, potentially accelerating degeneration. As a result, orthopedic strategies increasingly focus on preserving meniscus structure and supporting long-term joint function.
Degeneration in joint tissues may occur gradually over time, much like the age-related changes seen in thinning skin or reduced muscle tone. In many cases, care strategies focus on supporting the function of these tissues rather than removing them.
For example, physical therapy and nutritional interventions may help maintain muscle strength and joint health. Similarly, orthopedic interventions such as hyaluronic acid injections are designed to support joint function without removing tissue.
Ongoing research continues to explore methods that promote joint health by addressing cellular decline in orthopedic tissues.
Procedures using Regenexx lab processing utilize high concentrations of a patient’s own orthobiologic material. Physicians in the licensed Regenexx network use image-guided techniques to deliver the injectate precisely to targeted areas, with the goal of supporting joint function and mobility.
For individuals considering alternatives to surgery, a consultation with a physician in the licensed Regenexx network can help determine if these options are appropriate.

Medically Reviewed By:
